This Is Your Circulatory System | Part 2
The most common disorders of the circulatory system and their risk factors explained.
Welcome to The Feel Good Life! A newsletter about health, prevention, empathy and hope. I’m currently writing a brand new series called Basics Matter—in which we are exploring one human system per month for six months. This series is of free access to everyone. If you’re new around here, you can get started with the series right here.
A special note: On average, every newsletter in this series takes me around 25 hours of reading, researching, writing, and editing. I really hope you find immense value in this content, aimed to help you improve your own health. If you ever feel like upgrading to support this work, I’d highly appreciate it! Thanks in advance.
Hello again!
Dr. Mariana here, coming to you today with a really cool and in-depth learning to continue the second leg of our journey through the circulatory system.
In part 1 of the circulatory system we learned the basic structure (anatomy) and functioning (physiology) of the circulatory system—the marvellous plumbing network of your body. I also gave you some practical visuals to help you better grasp all these medical concepts, so that you can apply them as you learn to understand your body and recognise what it tells you. The communication and insights you get from your body are quite real, and they can be literally life-saving.
(Btw: did you watch Fantastic Voyage? I’m curious!)
Today we are diving into the other side of your circulatory system: the sickness side of it, also known as pathophysiology. We will talk about cardiovascular disease (CVD), global statistics, the biggest CVD risk factors, and the most common symptoms that people experience.
In today’s email you will learn:
What is Cardiovascular Disease (CVD)?
What are the most common cardiovascular diseases?
How does stress, high blood pressure and high cholesterol affect the circulatory system?
What are the most common risk factors and symptoms for CVD?
February is Heart Health Month!
It’s no coincidence that in February we have been learning everything about heart and vascular health. My intention is for you to better understand what happens in your body when circulatory disease develops, and most importantly, to show you how you can prevent for the future. So, we’re perfectly on time as we honour this vital system of the human body.
What Is Cardiovascular Disease?
When we talk about health problems in the circulatory system (also known as the cardiovascular system), we refer to them as Cardiovascular Disease (CVD)—simply an umbrella term to refer to the group of disorders of the heart and the blood vessels.
Cardiovascular disease affects more specifically the heart and the arteries, and not the veins. However, we will mention some of the most common vein problems as well.
A person can have symptoms of a cardiovascular disease, or no symptoms at all. Hence why it’s so tricky and risky. It can affect anyone regardless of their age, sex, ethnicity, or socioeconomic level.
As NHS explains:
“Cardiovascular disease (CVD) is a general term for conditions affecting the heart or blood vessels. It's usually associated with a build-up of fatty deposits inside the arteries (atherosclerosis) and an increased risk of blood clots. It can also be associated with damage to arteries in organs such as the brain, heart, kidneys and eyes.”
Disease in the circulatory system can happen indeed at any level. There are many types of CVD according to their location and cause:
Coronary heart disease – disease of the blood vessels supplying the heart muscle.
Cerebrovascular disease – disease of the blood vessels in the brain.
Peripheral arterial disease – disease of blood vessels in the arms and legs.
Rheumatic heart disease – damage to the heart muscle and heart valves from rheumatic fever, caused by a bacteria called Streptococcus.
Heart valve disease – disease in the heart valves resulting from anatomical problems, infectious disease or birth defects.
Congenital heart disease – birth defects that affect the normal development and functioning of the heart.
Deep vein thrombosis and pulmonary embolism – blood clots in the leg veins, which can travel to the heart and lungs.
Irregular heart rhythms
Today we will focus on the most common cardiovascular diseases, showing you how and why they happen, what factors are closely related, and how lifestyle changes can really impact your circulatory system’s health in the long run.
Cardiovascular Disease in Numbers
Did you know that cardiovascular disease is the world’s number one killer?
Sounds harsh but it is true…
Cardiovascular disease is the silent pandemic.
Disease in the circulatory system is the leading cause of death in the world—exactly a 31% according to the World Heart Federation and WHO. In fact, the most common causes of death globally (in this particular order) are:
Cardiovascular Disease (CVD)
Cancer
Chronic Respiratory Disease
In this report from 2022, Deloitte explains: ‘The World Health Organization (WHO) has reported that 17.9 million people died from CVD in 2019, translating to 31 percent of all deaths. More than 75% of CVD deaths occur in low- and middle-incomes countries and 85% of deaths are caused by heart attack and stroke.’
These numbers are a global reality, coinciding with data from numerous countries who have studied their own cardiovascular disease incidence.
In Australia in 2022, an estimated 1.3 million people aged 18 and over (6.7% of the adult population) reported having one or more conditions related to heart, stroke, or vascular disease.’
In China, ‘it is estimated that approximately 330 million individuals in China are affected by CVD, including 13 million strokes, 11.39 million coronary heart disease, 8.9 million heart failure, 5 million pulmonary heart disease and 245 million hypertension cases. In 2019, CVD accounted for 46.74% and 44.26% of all deaths in rural and urban areas, respectively. Two out of every five deaths are due to CVD.’
In the UK, over 7.6 million people have heart or circulatory diseases. It is a significant cause of disability and death, responsible for one in four premature deaths in the UK.
In the USA, ‘cardiovascular disease (CVD) remains the leading cause of death, claiming the lives of nearly 702,880 people in 2022, or about 1 in every 5 deaths.
If you are into data and statistics, here’s the full World Heart Report from 2023 with comprehensive info, graphics and maps, showing the severity of this silent pandemic.
As expected, all this data confirms what we already know thanks to decades of scientific research and medical analysis: cardiovascular disease is the most common, lethal, and persistent condition that is threatening human life.
Thankfully, with the body’s marvellous biology and a person’s conviction, awareness, and discipline, it is possible to practice lifestyle changes, helping prevent and avoid cardiovascular damage.
In order to do this, we need to talk about the most common risk factors. This will help you monitor yourself and decide where is it that you might need to take preventive action.
Most Common Risk Factors For Cardiovascular Disease:
Hypertension (High Blood Pressure)
Hypercholesterolemia (High cholesterol in the blood)
Obesity
Type 2 Diabetes
Smoking or Vaping
Harmful alcohol intake
Lack of physical activity
Genetics
It’s an undeniable truth that cardiovascular disease is a worldwide problem. Many factors are involved, from genetics to lifestyle choices, but what has truly modified all cardiovascular health for worse over the course of the years is this: the rushed pace of modern society.
The increasing amount of stress since the 1980’s, has severely impacted people’s health and wellbeing. Modern living has come at a high health cost. Despite the great advancements in technology and education, the increased sedentary lifestyles, processed foods, and stress, has significantly impacted health, leading to a rise in chronic diseases like obesity, diabetes, and cardiovascular issues, while also affecting mental well-being.
It’s then no surprise that the top 3 relevant risk factors for cardiovascular disease currently are:
Stress
High blood pressure
High cholesterol
Because they are the top 3 risk factors threatening your life, we need to have a good talk about them. Understanding how they affect your body, will be the foundation to understand and start making changes towards better health.
Let me show you how stress, high blood pressure, and high cholesterol can impact your cardiovascular health.
How Does Stress Affect The Circulatory System
Stress is the headmaster of cardiovascular disease.
When the body is under stress, hormones called cathecolamines are released by the adrenal glands (very tiny glands on top of your kidneys) into the bloodstream. These hormones are in charge of allowing your body work properly under stressful situations, making the heart beat faster, raising blood pressure, releasing sugar into the bloodstream—all things that the body needs in order to survive in an emergency situation. In essence, cathecolamines are in charge of the body’s fight-or-flight (stress) response.
In short-term stress, these hormones respond to a threat, allowing the body to react to protect itself. After the situation is under control, these hormones go back to normal.
In long-term stress however, the constant input of cathecolamines and their harmful effects, causes the body to develop chronic peaks of high blood pressure, blood sugar, and inflammation factors in the circulatory system. The body is great at adapting but it has its limits, as it’s only natural.
Two main cathecolamines in the body are Cortisol and Adrenaline—you might have heard of them. They are fascinating hormones, but when they have to keep working extra hours for months and years nonstop, its only expected that the system (your body) will start showing signs of exhaustion and wear.
When chronic stress happens, the body will develop chronic inflammation.
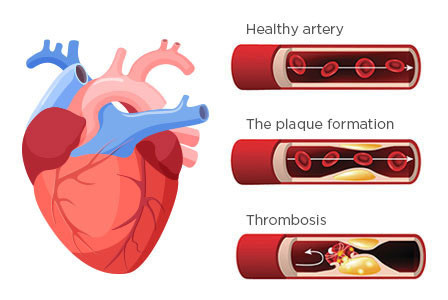
In the case of cardiovascular diseases, inflammation can show up as Atherosclerosis—a disease where fat builds up in the inner wall of arteries. This fat buildup is called a plaque or atheroma.
In the image below, see how the fat buildup (yellow) accumulates within the artery’s wall, narrowing the space and making it more difficult for blood to flow.
When there’s a blood vessel injury near a plaque, the immune system sends molecules and repair cells to the affected area. The blood vessels must widen up and become ‘leaky’ to let immune defense cells go through. In this leaky state of a blood vessel, the adjacent plaque becomes weak…risking the plaque to break from the wall, generating a blood clot that can fall into the bloodstream and block blood circulation, or travel places. This blockage can happen in the coronary (heart) arteries, causing a heart attack, or in the brain, causing a stroke. When a broken plaque travels through the bloodstream is what we call a thrombosis.
Here’s a 1-minute video explanation by the British Heart Foundation, showing how these fatty buildups or plaques happen and how they can affect your health:
Let’s not forget that chronic stress also affects our emotional and psychologic states, generating more hormonal input and sometimes leading to more inflammation in the body. Dr. Lampert, Yale University cardiologist explains:
‘When people feel they cannot escape the circumstances of their chronic stress, they may cope by turning to unhealthy behaviors,” says Gaffey. “We know that stress is associated with behaviors such as unhealthy diet, smoking, and increased use of alcohol.” These behaviors can lead to such health issues as high cholesterol and hypertension, which are primary risk factors for heart disease, she adds.’
How Does High Blood Pressure and Cholesterol Affect The Circulatory System?
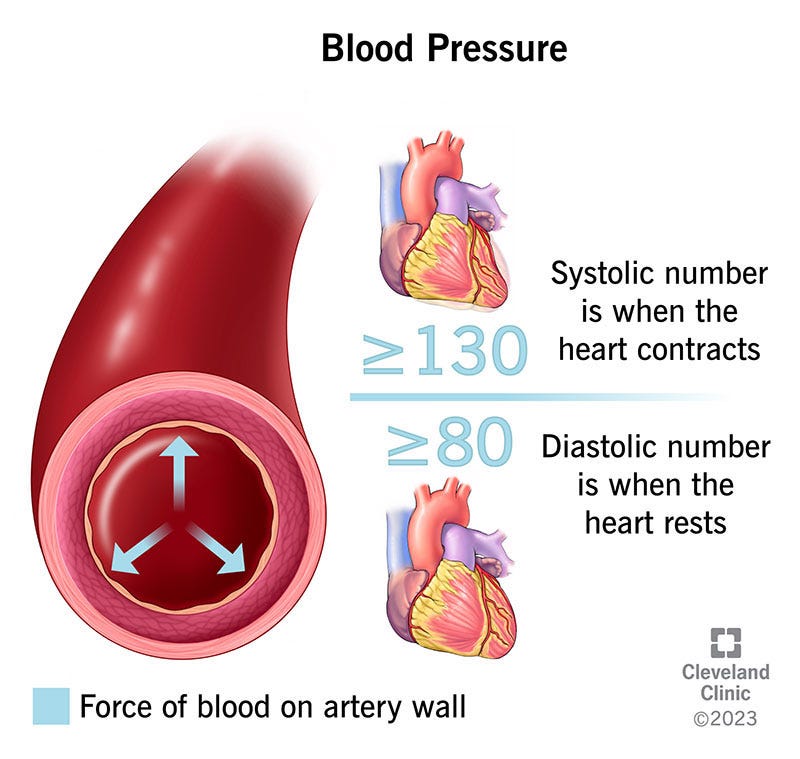
By definition, blood pressure is ‘the force of your blood pushing against the walls of your arteries as the heart pumps blood around your body.’ It is measured in millimeters of Mercury (mmHG) and expressed in two numbers, like this: 120/70 mmHg. The above number is called systolic pressure and the bottom one is called diastolic pressure. Systolic refers to the moment when the heart’s muscle contracts, pushing blood out through arteries. Diastolic is when the heart’s muscle relaxes, allowing the heart chambers to fill up again.
In a healthy adult, an average and healthy blood pressure should be between 90-130/60-80 mmHg.
When blood pressure is high, there can be symptoms or no symptoms at all. In fact, in most early cases there are no symptoms, hence why high blood pressure is considered the real silent killer. There can be peaks related to a stressful moment and temporary worries, which is only natural. But when chronic, the body adapts to the point where no symptoms will be felt for years.
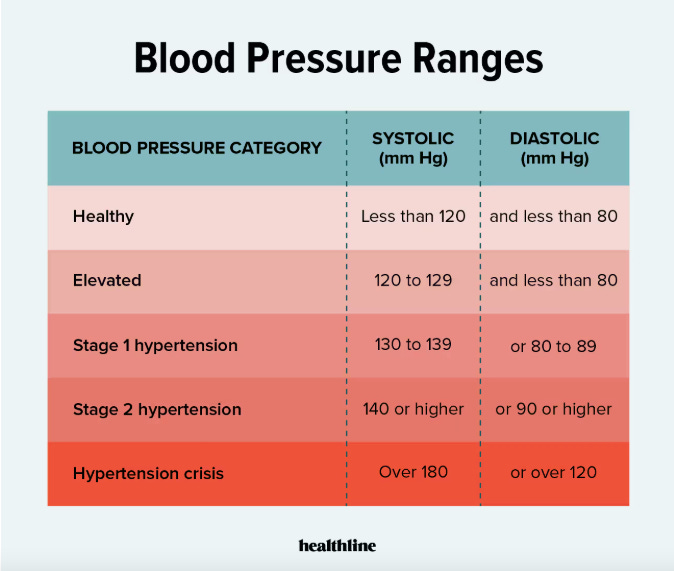
When blood pressure becomes chronically high, we call it Hypertension. It’s a full medical diagnose (that can only be done by a medical practitioner) and is one of the top 3 cardiovascular disease risk factors.
On the other hand, when blood pressure is low it’s called Hypotension, generally defined as a reading below 90/60 mm Hg. It is usually an acute event that will make a person feel weak, sweaty, dizzy, clouded and even faint. Sometimes it can be life-threatening.
It has many different causes including: emotional stress, fear, pain (the most common causes of fainting), as well as dehydration or certain medications.
The most recent Cardiology guidelines (2024) have established the key points for management of elevated blood pressure and hypertension, considering the risk factors in each case.
The updated guideline for blood pressure ranges are as shown here:
Let’s now talk about cholesterol.
Cholesterol is a waxy, fat-like substance that your body needs for good health (in the right amounts). It is in fact a particle of fat produced in the liver, that travels into and through the bloodstream attached to proteins called Lipoproteins. These lipoproteins can be of low density (LDL), very low density (VLDL), or high density (HDL). They help transport cholesterol in the blood.
Your liver produces all the cholesterol you need. The remainder comes from the food you eat, either from animals (dairy products and poultry), or from processed foods, which tend to contain saturated and trans fats (like palm oil)—not good for you. Most industrial foods these days use oils containing highly saturated fats, making it difficult to lead a cardiovascular protective diet.
When it comes to cholesterol, we must understand several things:
Cholesterol is not inherently bad for you. Cholesterol in the body is needed for many important things: it helps build every cell’s membrane; it is used to produce hormones, vitamin D, and bile (essential fluid for digestion). What’s bad is an excess of cholesterol.
There are different types of cholesterol, based on the lipoprotein they’re attached to. As mentioned, there is LDL, HDL, and VLDL cholesterol. LDL, commonly referred to as the “bad cholesterol”, is the one accumulating in plaques (the fat buildup in the walls of arteries), creating high risk for cardiovascular disease. HDL is the “good cholesterol” because it helps clear the bad cholesterol from the bloodstream by taking it back to the liver. HDL cholesterol is like the cleaning truck guys on the streets.
Whenever you get a cholesterol blood test, let your doctor analyse it for you. There are many factors that we take into consideration when analysing a full blood work, including physical examination and a medical history questionnaire. It’s not just numbers but an entire biochemical machinery that we are studying when interpreting your blood test. Be patient, get well-informed, and ask questions. Just don’t jump into conclusions on your own.
In the video below, you’ll find a wonderful explanation by the NIH of both good and bad cholesterol and how they relate to atherosclerosis, plaque in the arteries, and cardiovascular disease. It’s the perfect summary to this first section of today’s newsletter.
As with everything in life, excess is never good. Very high cholesterol will undoubtedly accumulate on your arteries’ walls, increasing your risk of a heart attack, a stroke and more. All this can be checked through routine blood tests that your doctor can request accordingly. If you are unsure if your cholesterol levels have been checked, or if you know of family history related to cholesterol or cardiovascular problems, please consult with your doctor.
Most Common Cardiovascular Diseases (CVD)
Now let’s dive properly into the disease side of the circulatory system.
As you might recall, the circulatory system has three main parts (heart, blood vessels and blood). We are going to study CVD focusing on the heart and blood vessels. While blood disorders can have cardiovascular implications, they are not inherently cardiovascular diseases themselves. We will study them later on in the series when we go into the realm of Haemotology (medical branch which studies blood disorders).
I will talk about the most important cardiovascular diseases without being too complex or extensive, so that you can really grasp the main concepts, to help you take good care of yourself and your beloved ones.
The most common cardiovascular diseases are:
Coronary Heart Disease (*Most common form of CVD)
Atherosclerosis (Cholesterol plaques in the arteries’ walls)
Cerebral Vascular Disease
Peripheral Vascular Disease
Strokes and TIA’s
Heart Failure
Aortic Disease
Valve Disease
Arrhythmias
Congenital Heart Disease
Most common cardiovascular symptoms:
Heart symptoms:
Chest pain (angina) - can be a dull, sharp, stabbing or aching pain
Chest pressure - more like an elephant foot’s pressing down on your chest
Pain or discomfort in the jaw, neck, arm or shoulder
Shortness of breath (dyspnea) - during activity or at rest
Dizziness, weakness, or lightheadedness
Fatigue or exhaustion
Nausea or vomiting
Cold sweat
Blood Vessel blockage symptoms:
Leg pain or cramps when walking
Changes in the skin on legs (cool or red areas)
Swelling on limbs
Coldness on limbs
Slow-healing wounds
Numbness (generalised or one-sided)
Weak peripheral pulse
Difficulty to talk, walk, see, or speak
Let’s break these Cardiovascular Diseases down—not like plaques though 😅 (pun intended!)
Coronary Heart Disease (CHD)
This is the most common form of cardiovascular disease—also known as Coronary Artery Disease (CAD) or Ischemic heart disease. It’s what most people mean when they say “heart disease.
To put you in context first, Coronary is the medical term relating to the arteries which surround and supply the heart with oxygenated blood.
Coronary heart disease is when your coronary arteries become narrowed by fatty material within their walls. Through the coronary arteries is how your heart’s muscle receive oxygen supply. When fatty material (plaques—also called atheroma) build up inside the coronary arteries walls, there’s a high chance that arteries will become so narrow that blood won’t be able to flow through them, causing a blockage and limited or no oxygen supply, and with it, a heart attack.
This atheroma plaques will cause arteries to narrow and harden up. This is what we call Atherosclerosis (as explained earlier) and it’s one of the main risks factors for Coronary Heart Disease.
You might have coronary heart disease for many years and not have any symptoms until you experience a heart attack. Again, that’s why coronary disease is a “silent killer.”
When symptoms do appear, is common to feel chest pain, neck/jaw/left arm pain or numbness, dizziness, sweating, heartburn, nausea, vomiting, and/or fainting. In any of these cases, always contact your healthcare provider or emergency service immediately.
To learn more about Coronary Heart Disease, read here, here and here.
Cerebrovascular Disease
This is an umbrella term that refers to conditions affecting the brain's blood vessels and blood supply, including stroke, transient ischemic attacks (TIAs), aneurysms, and vascular malformations. These are usually medical emergencies and require urgent evaluation and treatment.
The most common cerebral blood vessels affected are the Carotid arteries, located in the neck on the way up to your brain, and Vertebral arteries, part of the Willis Circle as we studied in Nervous System Part 2.
Stroke: The most common cerebrovascular disease. They happen when a blood clot or broken vessel prevents blood from getting to your brain, leading to damaged tissue affecting the affected area’s functions (speech, movement, memory, just to mention a few). Strokes are considered a medical emergency as they could be fatal. When immediate attention is received, there are good chances for diagnose, treatment and recovery.
The American Stroke Association suggests the acronym F.A.S.T to detect symptoms of a stroke:
TIA: A transient ischemic attack (TIA) — sometimes called a “mini-stroke” — is like a stroke, but the effects are temporary, usually resolving within 24 hours. It’s often a warning sign that a person has a very high risk of having a true stroke soon. It’s always advised to get immediate medical attention to rule out other possible major problems. For more info on TIA, you can read here.
Aneurysms: bulges or ballooning that form due to weakening of the walls in blood vessels (most common in arteries), which can rupture and cause bleeding in the brain. After formed, aneurysms can continue to grow, increasing chances of rupture. Treatment will always focus on preventing rupture. Other places where aneurysms can happen besides the brain are in the aorta, kidneys, intestines, spleen, and larger vessels in the legs. In the brain, they can cause headaches, but it’s not uncommon for a small aneurysm to go unnoticed and without symptoms for years. In fact, they tend to be a casual finding when doing other imaging studies. To learn more about aneurysms, read here.
Vascular Malformations: abnormal growths of blood vessels or lymphatic vessels that can occur anywhere in the body, often present at birth, and may cause cosmetic or functional problems. Usually benign. To learn more about vascular malformations, read here.
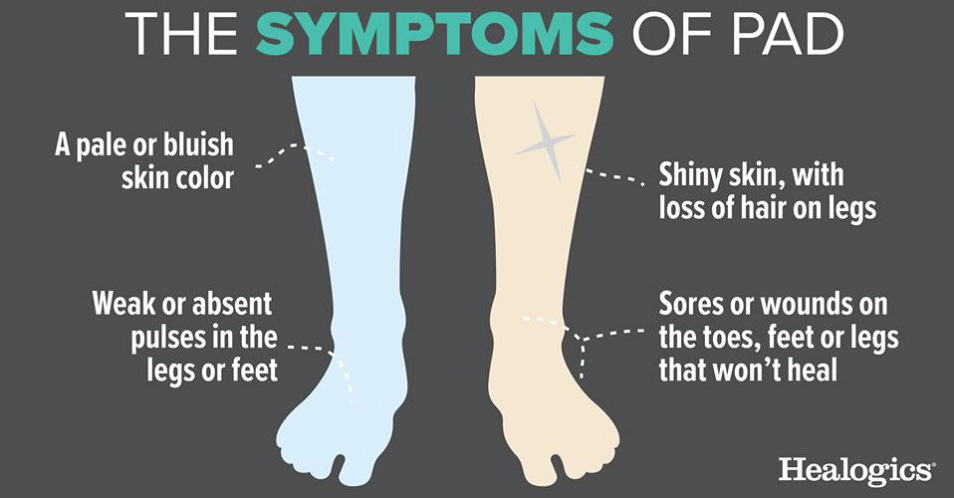
Peripheral Artery Disease (PAD)
This refers to the accumulation of plaque (fats and cholesterol) in the arteries in your legs or arms, making it harder for your blood to carry oxygen and nutrients to the tissues in those areas—very similar to coronary artery disease. The most common symptoms in legs include cramping, fatigue, and pain when doing physical activity, like walking—this is called Claudication.
The strongest risk factors are diabetes and smoking. The good news is that it can improve through exercising, eating less fat, and giving up tobacco products. If left unattended, this peripheral vascular disease can lead to severe localised infections like gangrene and amputations. The medical specialist in charge of evaluating peripheral vascular problems is the Vascular Surgeon.
To learn more about PVD, read here.
Aortic Disease
Aortic disease are disorders and conditions affecting the Aorta, the most important artery carrying blood from the heart to the entire body. Aortic disease happens when the walls of the aorta become weak and bulge, split, burst or block up. These are very serious and life-threatening conditions and require immediate attention. Luckily, they’re not as common. It’s usually recommended to perform an ultrasound screening in men 60 and older who have ever smoked or used tobacco products, and for people who have a family history of aneurysm. If you or someone you know fall in any of these categories, please ask your doctor to see if screening might be advised.
To learn more about aortic disease, read here.
Heart Valve Disease
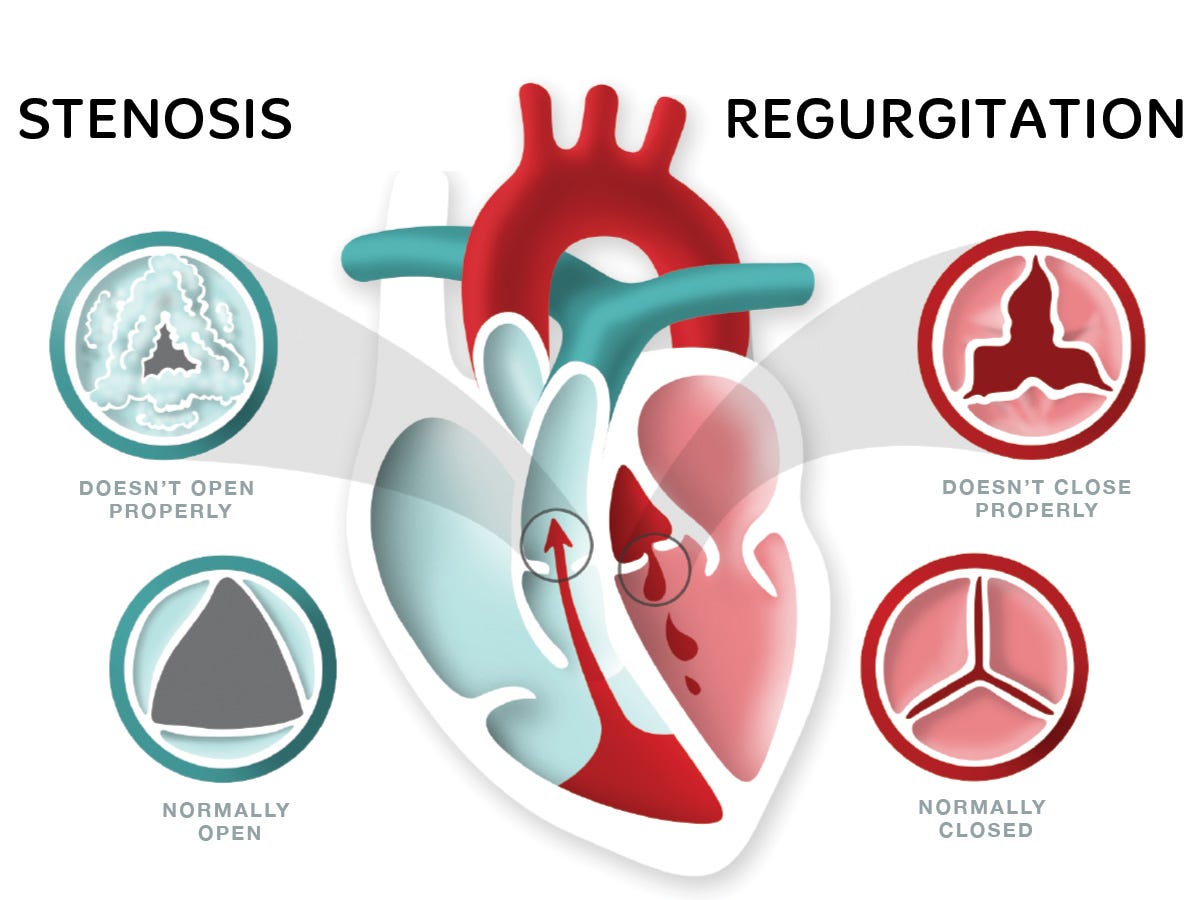
Heart valve disease is where one or more of the valves in your heart (4 in total) does not work as it should, keeping your blood from flowing in one direction through the heart. Common types of heart valve disease include narrowing (stenosis), backward flow (regurgitation) or stretchy, floppy leaflets that don’t close tightly (prolapse).
Heart valve disease don’t always give symptoms, but when they do, a person can experience shortness of breath, dizziness, weakness, palpitations, swollen ankles, or chest discomfort. If unattended, it could lead to heart failure. Treatment options can include medication, valve repair or replacement. If you experience any of these symptoms, always consult with your doctor.
Heart valves can also be affected by infections, particularly after certain throat infections by specific bacteria that can travel to the heart (e.g. rheumatic heart disease), or after a valve replacement. Medical monitoring by multiple specialists is often required.
To learn more about heart valve disease, read here.
Arrhythmias
An arrhythmia is an irregular heartbeat, making the heart beat too slowly, too quickly, or irregularly. This happens due to altered electric signals in the heart’s pacemaker (Sinoatrial Node), chemical imbalances, infections, medications, drugs, alcohol, smoking, caffeine, and/or stress. Arrhythmias can be temporary or permanent; they can be present at birth or develop throughout life. They may feel like a fluttering, pounding or racing heartbeat. While some heart arrhythmias are harmless, others may cause life-threatening symptoms.
To give you a general overview, the normal heartbeat rate varies with age:
babies (birth to 3 months of age): 100–150 beats per minute
kids 1–3 years old: 70–110 beats per minute
kids by age 12: 55–85 beats per minute
age 12 and onwards: 60-100 beats per minute
There are many types of arrhythmias. Any unusual sensations should always be checked by a Cardiologist (heart specialist) who will use different techniques to study your heart and make a proper diagnose, and prescribe medications if needed.
To learn more about arrhythmias, read here.
Heart Failure
It’s a heart condition where it can’t pumping enough blood to meet the body’s blood and oxygen requirements. causing tiredness and shortness of breath. This can also cause a fluid buildup in the body, showing up as swollen legs or feet, making it harder to breathe. Heart failure is a chronic condition, but with proper medical control, treatment, and lifestyle changes, a person can lead an active life.
To learn more about heart failure, read here.
Congenital Heart Disease
Congenital heart disease is one or more problems with the heart's structure that are present at birth. Congenital means that you're born with the condition. Some issues are more severe than others, but all of them prevent normal blood flow through your heart and beyond. These congenital problems can include: having a hole in the heart’s wall, blood vessel or valve problems.
It’s common to have congenital heart disease associated with other congenital problems. Sometimes they might show early symptoms, or no symptoms at all until later in life. Risk factors for congenital heart disease include: genetics, rubella, diabetes, smoking, alcohol, and certain medications. It’s important that during pregnancy, women get proper medical control and regular checkups. When congenital diagnoses appear later in life, is equally important to consult and keep medical checkups.
To learn more about congenital heart disease, you can read here.
Pericarditis
Pericarditis is the inflammation of the sack that protects the heart, called Pericardium. It has two layers and when they get irritated, they swell and rub against each other, causing a sharp or stabbing pain in the chest. Pericarditis is often mild, sometimes resolving on its own, or with help of medication if needed. This can be a one-time event or a recurrent event. It’s always important that over any chest pain sensation, you consult your doctor without delay.
To learn more about pericarditis, read here.
Deep Vein Thrombosis (DVT)
Deep vein thrombosis is a blood clot in one or more veins, usually in the legs. It can cause leg pain or swelling. Sometimes there are no noticeable symptoms. It’s a dangerous, life-threatening condition, mostly because a clot in the vein will travel back to the lungs and the heart, potentially affecting breathing and proper heart circulation. The most common symptoms are:
Throbbing pain in 1 leg (rarely both legs), usually in the calf or thigh, when walking or standing up
Swelling in 1 leg (rarely both legs)
Warm skin around the painful area
Red or darkened skin around the painful area – this may be harder to see on brown or black skin
Swollen veins that are hard or sore when you touch them
These symptoms can also happen in your arms or belly as clots can happen in those areas too. When a clot travels through the bloodstream into the lungs, a person can experience shortness of breath and chest pain. Always consult your doctor or an emergency service as needed.
To learn more about deep vein thrombosis, read here.
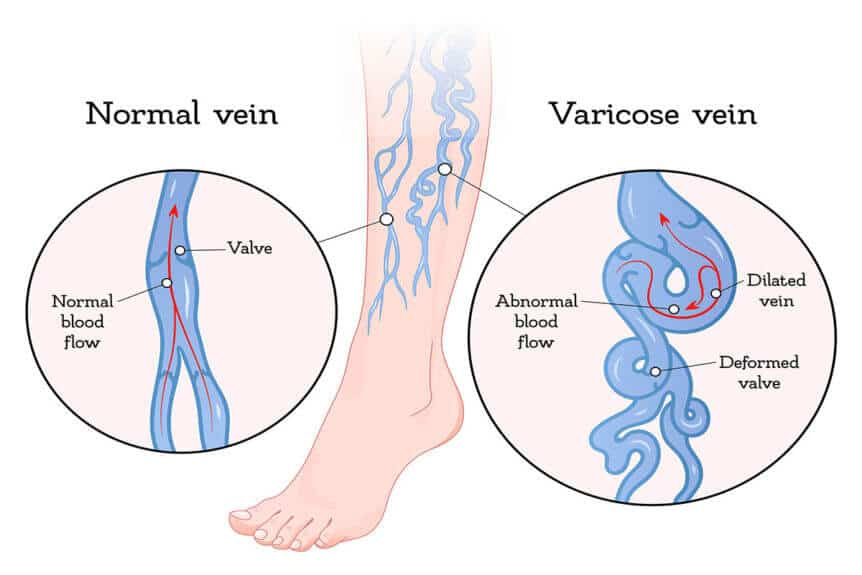
Varicose Veins
Even though they are not a cardiovascular disease, varicose veins are a common affection of the circulatory system. Varicose veins are enlarged, bulged veins that can happen anywhere in the body, but more commonly in the legs. This happens when the valves in the veins or their walls become weak, forming bulges where blood can sit or flow backwards. This can also come as a result of increased pressure in the veins due to long periods of standing or sitting, obesity, and pregnancy.
Varicose veins are usually seen near the skin’s surface, and depending on their level of affection, they can even be felt like a chain of little lumps (like a rosary) that follows a vein’s path. When this happens, the circulatory system has to create parallel circulation pathways to assure that blood can return to the heart as normally as possible. In some cases, spider veins are a result of this parallel circulation system due to veins with weak valves or walls.
If you worry about how your veins look and feel, and self-care measures haven't helped, see your healthcare professional about them.
To learn more about varicose veins, read here and here.
Vasculitis
Vasculitis is the irritation, swelling and inflammation of blood vessels. The inflammation can cause a vein’s wall to thicken, harden and narrow, affecting the blood flow. It can happen anywhere in the body, and they’re mostly seen in autoimmune disorders—where an unexpected response by your body’s immune system causes it to attack your blood vessels. Autoimmune disorders such as Lupus, Rheumatoid Arthritis, Scleroderma, Behcet, and Kawasaki diseases can lead to vasculitis. Causes are unknown; thankfully they are rare.
To learn more about vasculitis, you can read here, here and here.
Now, after having learned in depth about the main cardiovascular diseases and their risk factors, you have all the tools to know what are the things you might be at risk of, things to start observing in your routine, and things you could fix in your lifestyle to help your health and body improve, starting now.
Tomorrow, we will talk about the final (and most important) part in this circulatory system chapter: PREVENTION. I will give you a comprehensive list of good practices and preventative tips to help you start taking good care of your cardiovascular health.
For now, take the time to digest today’s learning. 😉
Let’s Summarise
In today’s chapter, you have learned:
When the circulatory system gets sick, we can have heart problems, artery problems, and vein problems. They can happen at any level in the body, and for all sorts of reasons.
Cardiovascular disease is the #1 cause of death worldwide. Also known as the silent killer.
The most common form of cardiovascular disease is coronary heart disease, related to problems in the circulation and blood flow that supports your heart.
The most common risk factors for cardiovascular disease are stress, high blood pressure, high cholesterol, and fat buildup in the arterial walls (plaques). Other equally important risk factors are obesity, diabetes, sedentarism, smoking/vaping, alcohol consumption, and genetics.
The most common symptoms of circulatory illness are shortness of breath, chest pain, chest pressure, dizziness, cramps, swelling in the legs, fatigue, and exhaustion.
*As always, if you have doubts or questions, leave them in the comment section so I can clear them out for you—and for everyone to learn from.
See you tomorrow on Part 3! The last of the Circulatory System: “Good Practices for Circulatory Health and Cardiovascular Disease Prevention.”
Much Love,
Dr. Mariana
If you found this content helpful, please ❤️ it and pass it around. Heart and vascular health are vital. Learning about it might just save someone’s life.
















Fascinating, clearly explained and highly useful information. Thank you Dr. M!